You're holding your newborn at the top of the stairs, and suddenly your mind flashes an image: What if I dropped them?
You're giving the baby a bath, and unbidden thought appears: What if I held their head underwater?
You're driving with your baby in the back seat: What if I swerved into oncoming traffic?
These thoughts are so horrifying that you can't tell anyone. You must be a terrible person. A dangerous mother. You should never be left alone with your baby.
Here's the truth that might save your sanity: 91% of new parents experience disturbing intrusive thoughts about their baby. You're not dangerous. You're not abnormal. You're experiencing one of the most common—and most silent—aspects of new parenthood.
This guide explains what's normal, what's not, and when these thoughts signal something that needs treatment.
What Are Intrusive Thoughts?
Intrusive thoughts are unwanted, disturbing thoughts or mental images that pop into your mind without your control. They're the brain's equivalent of spam emails—thoughts you didn't ask for, don't want, and don't reflect your true desires.
Common Postpartum Intrusive Thoughts:
Harm-related:
- Dropping the baby down stairs or from a height
- Baby suffocating or drowning during bath time
- Accidentally harming baby while using knives in kitchen
- Baby being harmed by household pets
- Sexual thoughts about the baby (extremely disturbing but not uncommon)
Catastrophic fears:
- SIDS scenarios playing on repeat
- Car accidents with baby in vehicle
- Baby being kidnapped or harmed by others
- Contamination fears (germs, chemicals, illness)
The key characteristic: These thoughts are ego-dystonic—meaning they're completely at odds with your values and desires. They horrify you because you would never want these things to happen.
Normal Intrusive Thoughts vs. Postpartum OCD
The difference isn't the thoughts themselves—it's your response to them and how much they interfere with your life.
Normal Postpartum Intrusive Thoughts:
The thought: "What if I dropped the baby down the stairs?"
Your response:
- "That was a weird thought. Anyway..." (dismiss and move on)
- Brief discomfort, but thought passes quickly
- Might be more careful on stairs, but not excessively so
- Thoughts are infrequent (few times a week)
- Doesn't significantly change your behavior
Postpartum OCD:
The same thought, but:
Your response:
- "Oh my God, why did I think that? Am I dangerous? What's wrong with me?"
- Spend hours ruminating about what the thought means about you
- Avoid stairs entirely, or only go up/down while someone else holds baby
- Thoughts are frequent (multiple times daily)
- Develop compulsive behaviors to "prevent" the feared outcome
- Experience significant anxiety and distress
The Postpartum OCD Cycle
- Intrusive thought appears: "What if I harm my baby?"
- Misinterpretation: "Having this thought means I might actually do it"
- Anxiety spike: Intense fear and guilt
- Compulsion: Ritual to "neutralize" thought or prevent harm
- Checking baby's breathing constantly
- Avoiding being alone with baby
- Removing all knives from kitchen
- Excessive cleaning/sanitizing
- Seeking reassurance repeatedly ("I'm not dangerous, right?")
- Temporary relief... then thought returns, cycle repeats
This is OCD—not because you're having disturbing thoughts (that's normal), but because the thoughts are creating a compulsive cycle that interferes with your life.
Postpartum OCD vs. Postpartum Psychosis (Critical Distinction)
This is the most important section of this article, because confusion between these two conditions causes unnecessary fear and prevents people from seeking help.
Postpartum OCD:
- Thoughts are unwanted and horrifying to you
- You're terrified you might act on them (but you won't and never have)
- You recognize the thoughts are irrational
- You avoid situations where intrusive thoughts occur
- You develop safety behaviors to prevent acting on thoughts
- You are not at risk of harming your baby
Postpartum Psychosis (extremely rare: 0.1-0.2%):
- Thoughts feel real and rational to you
- You may believe you should act on commands or delusions
- Hallucinations (hearing voices, seeing things that aren't there)
- Delusions (fixed false beliefs, like baby is possessed or evil)
- Confused thinking, disorganized behavior
- This is a psychiatric emergency requiring immediate hospitalization
If you're horrified by your thoughts, you have OCD, not psychosis. People with postpartum psychosis don't recognize their thoughts as disturbing—they believe them to be true.
Why Intrusive Thoughts Happen Postpartum
Neurobiological explanation:
Your brain's threat-detection system goes into overdrive after having a baby. This was evolutionarily adaptive—hypervigilance to danger kept babies alive.
But in modern life with low actual danger, this system misfires:
- Your brain constantly scans for threats to your baby
- It generates "what if" scenarios to prepare for danger
- These scenarios become intrusive thoughts
- Your horror at these thoughts proves you're not dangerous—you're hypervigilant
Hormonal factors:
- Dramatic drop in estrogen and progesterone after birth affects OCD-related brain circuits
- Sleep deprivation impairs the brain's ability to filter out unwanted thoughts
- Stress hormones increase "sticky" thinking (thoughts that won't go away)
When to Seek Help
Seek professional evaluation if:
- Thoughts are frequent: Multiple times per day, most days of the week
- Thoughts cause significant distress: Hours spent worrying about what thoughts mean
- You're developing compulsions:
- Excessive checking (baby breathing, locks, appliances)
- Avoiding being alone with baby
- Seeking constant reassurance
- Mental rituals (counting, praying, neutralizing thoughts)
- Interference with daily life: Can't complete basic tasks due to rituals or avoidance
- Impact on bonding: Avoiding holding or caring for baby due to intrusive thoughts
Treatment for Postpartum OCD
Exposure and Response Prevention (ERP) - Gold Standard:
ERP is a specific type of therapy that teaches you to:
- Exposure: Gradually expose yourself to situations that trigger intrusive thoughts (e.g., holding baby near stairs)
- Response Prevention: Resist performing compulsions (e.g., not checking baby 20 times after thought appears)
- Result: Brain learns thoughts are just thoughts, anxiety decreases, compulsion cycle breaks
ERP is highly effective: 60-80% of people experience significant improvement within 12-16 weeks.
Medication:
- SSRIs: Same medications used for depression/anxiety, but often at higher doses for OCD
- Safe while breastfeeding: Zoloft and Prozac have extensive safety data
- Timeline: 8-12 weeks to see full effects (OCD takes longer to respond than depression)
Self-Help Strategies:
1. Label thoughts accurately:
"This is an intrusive thought caused by my hyperactive threat-detection system, not a desire or intention."
2. Don't engage with thoughts:
- Don't try to analyze or figure out why you had the thought
- Don't seek reassurance ("I'm not dangerous, right?")
- Notice the thought, label it, move on
3. Resist compulsions:
- If you're checking baby breathing every 5 minutes, extend to 10 minutes, then 15
- Sit with the anxiety instead of performing the ritual
- Anxiety will peak and then naturally decrease
4. Sleep (if humanly possible):
- Sleep deprivation makes intrusive thoughts worse and harder to dismiss
- Partner night shifts, pumping to allow longer sleep stretches—whatever works
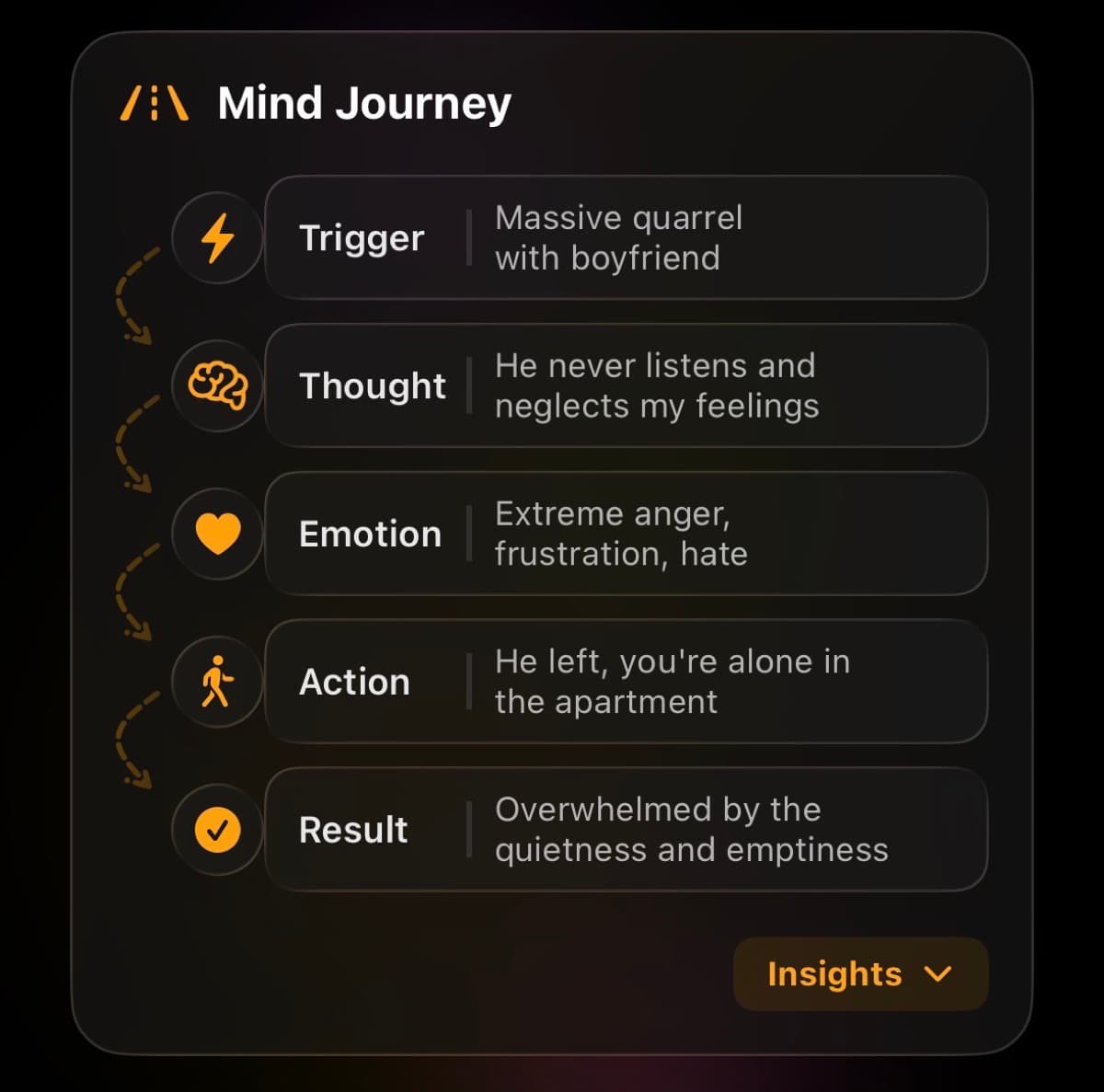
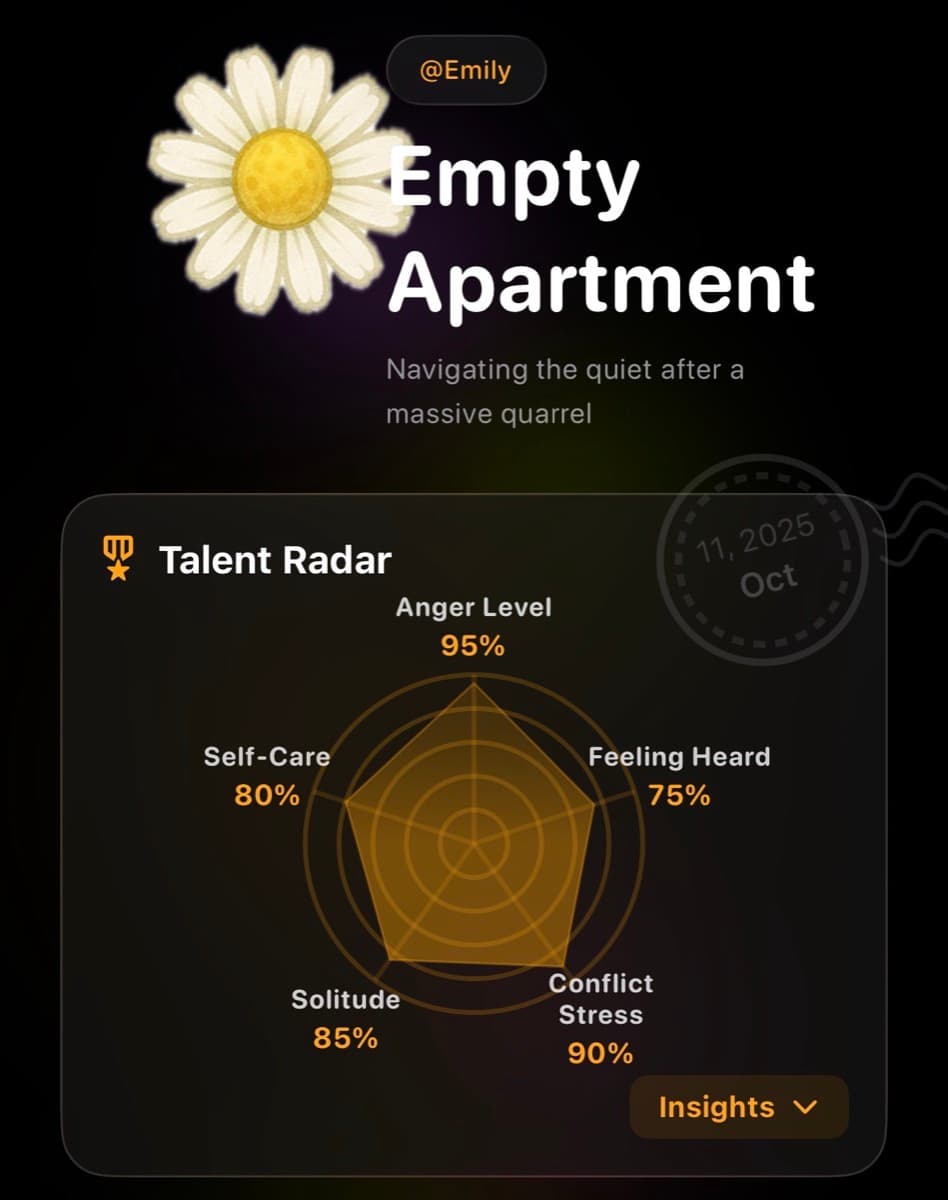
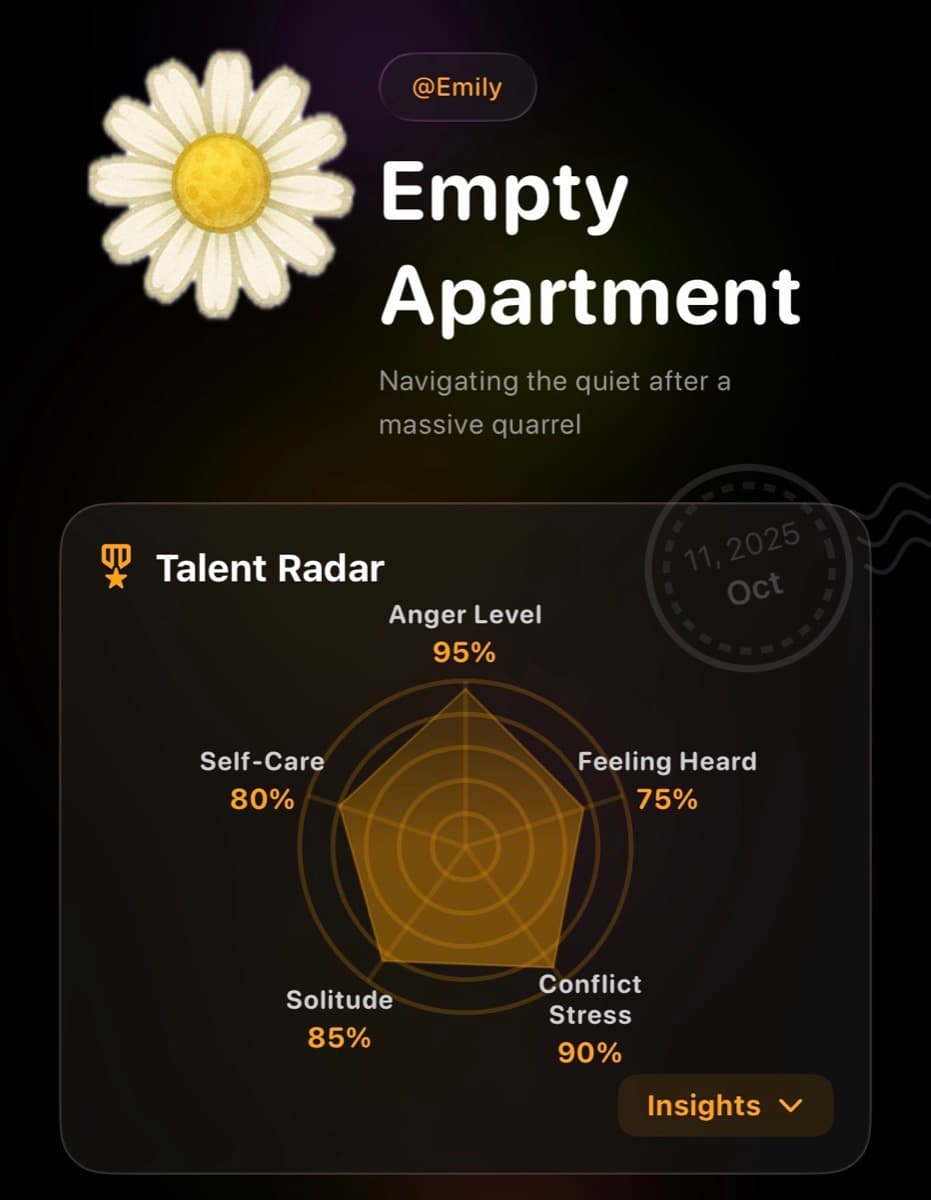
Using Lifelight for Intrusive Thought Tracking
One of the hardest parts of postpartum OCD is explaining it to your doctor in a 15-minute appointment. Lifelight helps you track and articulate patterns:
- Intrusive thought log: Track frequency, triggers, and your response (did you perform compulsion?)
- Anxiety tracking: Document how much distress thoughts cause over time
- Compulsion monitoring: Track ritual behaviors to see if they're increasing
- Treatment response: Monitor whether ERP or medication is reducing frequency/distress
- Private journaling: Write about disturbing thoughts you can't say out loud yet
When you show your doctor: "I'm having intrusive thoughts about harming my baby 15-20 times per day, and I've developed these checking rituals," you're much more likely to get appropriate OCD-specific treatment instead of generic anxiety advice.
What NOT to Do
Don't:
- Confess thoughts to partner/family repeatedly: This is a reassurance compulsion that makes OCD worse
- Try to suppress thoughts: "Don't think about pink elephants" → you immediately think about pink elephants. Same with intrusive thoughts.
- Avoid all situations that trigger thoughts: Avoidance maintains OCD; gradual exposure breaks it
- Assume thoughts mean something about you: They don't. 91% of new parents have them.
For Partners: How to Help
If your partner discloses intrusive thoughts:
- Don't panic: These thoughts are common and don't indicate danger
- Don't provide excessive reassurance: "You're not dangerous" once is supportive; 20 times becomes a compulsion
- Encourage professional help: "These thoughts are treatable. Let's find an OCD specialist."
- Don't take over all baby care: Avoidance makes OCD worse; gentle exposure helps
- Educate yourself: Understanding OCD helps you support effectively
The Timeline of Recovery
Without treatment: Postpartum OCD can persist for years, often transitioning into chronic OCD
With ERP therapy:
- Weeks 1-4: Learning to identify compulsions and resist them
- Weeks 4-8: Gradual exposure to triggering situations
- Weeks 8-12: Noticeable reduction in thought frequency and distress
- Weeks 12-16: Significant improvement; thoughts still occur but easy to dismiss
With medication + ERP: Often faster and more complete response than either alone
You Are Not Your Thoughts
The fact that these thoughts horrify you is proof you're not dangerous. People who actually harm their children don't have intrusive thoughts about it—they don't perceive the harm as unwanted or disturbing.
Your horror is your humanity. Your hypervigilance is your brain trying (too hard) to keep your baby safe. You're not broken. You're experiencing a treatable condition that affects millions of new parents.
These thoughts don't define you. They're noise, not signal. And with proper treatment, the noise gets quieter.
You're a good parent seeking help for a medical condition. That's exactly what your baby needs.