It's 4 AM. The baby has been awake every 90 minutes all night. You're so tired you can't remember if you fed them 20 minutes ago or 2 hours ago. You're staring at your partner, trying to form words, but your brain feels like it's moving through molasses.
You knew new parents were tired. Everyone told you. But nobody told you it would feel like this.
Nobody told you that sleep deprivation would make you:
- Cry over spilled milk (literally)
- Forget your own address when filling out forms
- Have intrusive thoughts about something happening to your baby
- Feel rage at your partner for breathing too loud
- Question whether you're capable of being a parent
Here's what nobody says: Extreme sleep deprivation isn't just exhaustion—it's a mental health crisis masquerading as "normal new parent life."
This guide covers the real effects of sleep deprivation, why it's so destructive to mental health, and evidence-based strategies that actually work (not the useless "sleep when baby sleeps" advice).
The Numbers Nobody Mentions
- New parents lose an average of 44 days of sleep in the first year
- Mothers average 5.1 hours of sleep per night in first 3 months (fragmented, not continuous)
- Sleep deprivation peaks at 3 months postpartum and can last until baby is 6+ months
- Fragmented sleep is worse than short sleep: 6 hours interrupted is more damaging than 4 hours continuous
For reference: Sleep deprivation is used as a torture technique because it reliably causes psychological breakdown. We're doing this to new parents and calling it "part of the journey."
What Sleep Deprivation Actually Does to Your Brain
Cognitive Effects:
- Memory impairment: Similar to having a blood alcohol level of 0.1% (legally drunk)
- Reaction time slows: Driving after 24 hours awake = driving drunk
- Decision-making deteriorates: Poor judgment, impulsivity, risk-taking
- Attention problems: Can't focus, easily distracted, difficulty completing tasks
Emotional Effects:
- Emotional dysregulation: Crying, rage, inability to control reactions
- Anxiety spikes: Catastrophic thinking, constant worry, panic symptoms
- Depression risk triples: Sleep deprivation is both symptom and cause of PPD
- Decreased stress tolerance: Small problems feel overwhelming
- Irritability: Snapping at partner, resentment, conflict
Physical Effects:
- Weakened immune system (more frequent illness)
- Increased cortisol (stress hormone)
- Weight gain and difficulty losing baby weight
- Decreased milk production (if breastfeeding)
- Higher blood pressure and diabetes risk
The Sleep Deprivation-Depression Spiral
- Sleep deprivation causes depressive symptoms: Hopelessness, emotional numbness, crying
- Depression causes insomnia: Even when baby sleeps, you can't
- More sleep deprivation worsens depression: Downward spiral accelerates
- Depression symptoms blamed on "adjustment": Nobody recognizes it as treatable condition
Breaking this cycle requires prioritizing sleep as aggressively as you'd treat any other medical emergency.
Why "Sleep When Baby Sleeps" Is Useless Advice
This advice sounds logical but ignores reality:
- Babies sleep in 2-3 hour chunks: Adults need 4+ hour blocks for restorative sleep
- You can't fall asleep instantly: By the time you fall asleep, baby wakes up
- Hypervigilance prevents sleep: You're listening for baby, can't fully relax
- Household tasks must happen sometime: When baby sleeps is often the only time
- You're not a robot: Can't switch sleep on/off on command
What actually works: Strategic sleep shifts that guarantee one 4-5 hour block of continuous sleep per person per night.
Evidence-Based Sleep Strategies That Actually Work
1. The Night Shift System
How it works:
- Partner A: 9 PM - 2 AM (5 hours continuous sleep)
- Partner B: 2 AM - 7 AM (5 hours continuous sleep)
- Partner on duty handles ALL wake-ups, other person wears earplugs + sleeps in different room if possible
If exclusively breastfeeding:
- Pump before your sleep shift
- Partner bottle-feeds during their shift
- Even 2-3 nights per week makes massive difference
If solo parenting:
- Trade sleep shifts with friend, family member, or paid night doula
- Even one 5-hour block per week improves mental health significantly
2. Prioritize Sleep Over Everything Else
What to deprioritize temporarily:
- Clean house (hire cleaning service if possible, or just lower standards)
- Home-cooked meals (prepared meals, takeout, simplest possible cooking)
- Hosting visitors (they can come back when you're sleeping)
- Responding to texts/calls immediately
- Any non-essential tasks
Repeat after me: "Sleep is more important than a clean kitchen. Sleep is more important than thank-you notes. Sleep is more important than appearing to have it together."
3. Understand Sleep Cycles and Architecture
Why this matters:
- One 4-hour continuous block > four 1-hour naps
- Deep sleep (first 3-4 hours) is when brain restores and processes
- REM sleep (later cycles) regulates emotions
- Interrupted sleep prevents deep sleep, even if total hours seem adequate
Strategy: Protect at least one continuous sleep block per night—this is non-negotiable for mental health.
4. Safe Co-Sleeping / Room-Sharing Optimization
If following safe sleep guidelines with baby in bassinet:
- Move bassinet away from your side during partner's sleep shift
- Use white noise to muffle baby sounds that aren't full cries
- Partner on duty sleeps on couch or different room with baby monitor
Goal: Off-duty parent cannot hear every snuffle and movement.
5. Sleep Hygiene (Even in Chaos)
- Blackout curtains: Sleep whenever you can, regardless of time of day
- White noise machine: For both baby and parents
- Cool room temperature: 65-68°F optimal for sleep
- Earplugs for off-duty parent: High-quality foam earplugs block baby sounds
- Magnesium supplement: Helps with sleep quality (check with doctor)
When Sleep Deprivation Becomes Dangerous
Seek immediate help if you experience:
- Microsleeps: Falling asleep for seconds while holding baby or driving
- Hallucinations: Seeing or hearing things that aren't there (can happen with extreme sleep deprivation)
- Intrusive thoughts about harming baby: Often worsened dramatically by sleep deprivation
- Inability to function: Can't complete basic tasks, forgetting to eat, dangerous mistakes
- Suicidal thoughts: Sleep deprivation can trigger severe depression
This is a medical emergency. Call your doctor, go to ER, or call Postpartum Support International: 1-800-944-4773
The Sleep Deprivation - PPD Connection
Research shows:
- Poor sleep in early postpartum period predicts PPD at 3 months
- Each additional night waking increases depression risk by 8%
- Improving sleep can reduce PPD symptoms by 50% within 2 weeks
- Sleep interventions should be first-line treatment before medication
If you're experiencing PPD symptoms, prioritizing sleep isn't luxury—it's treatment.
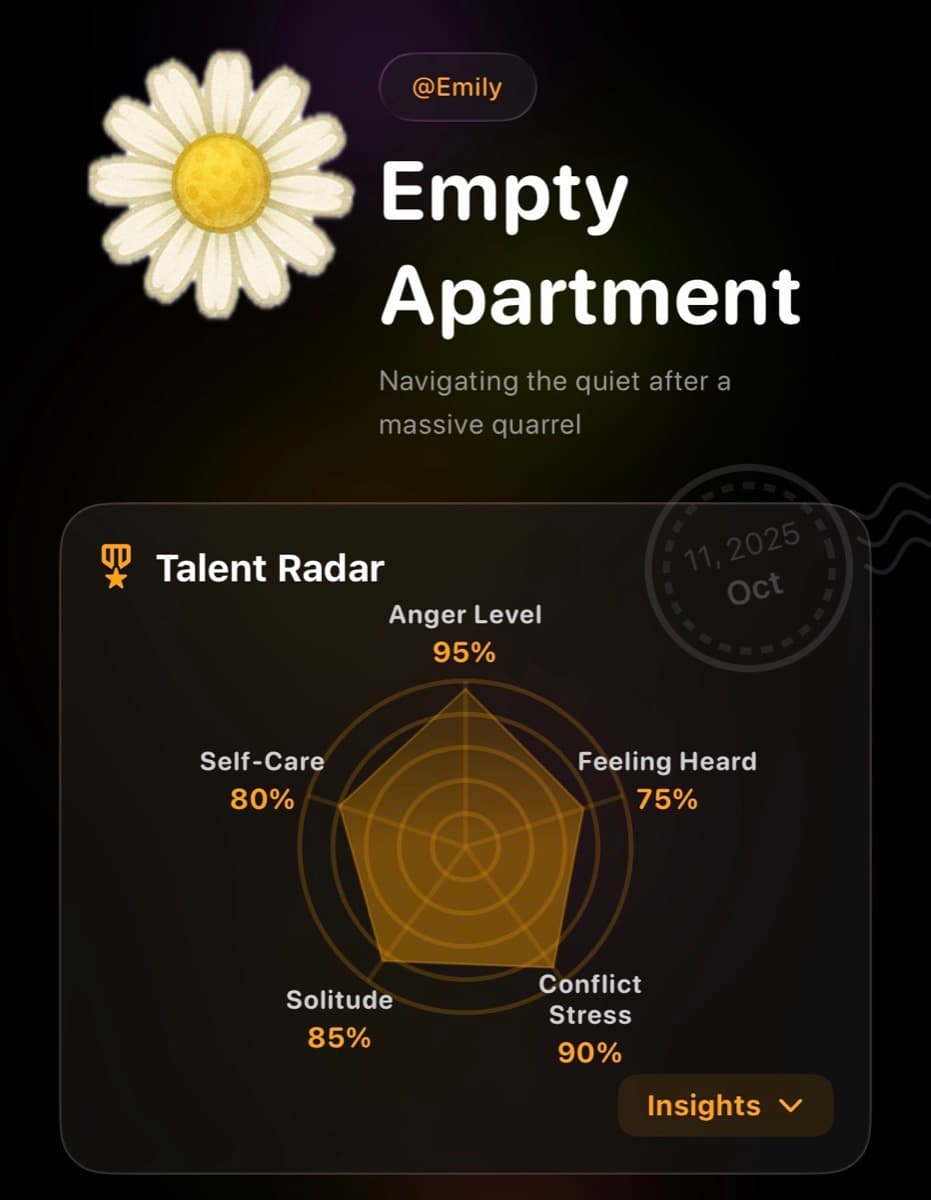
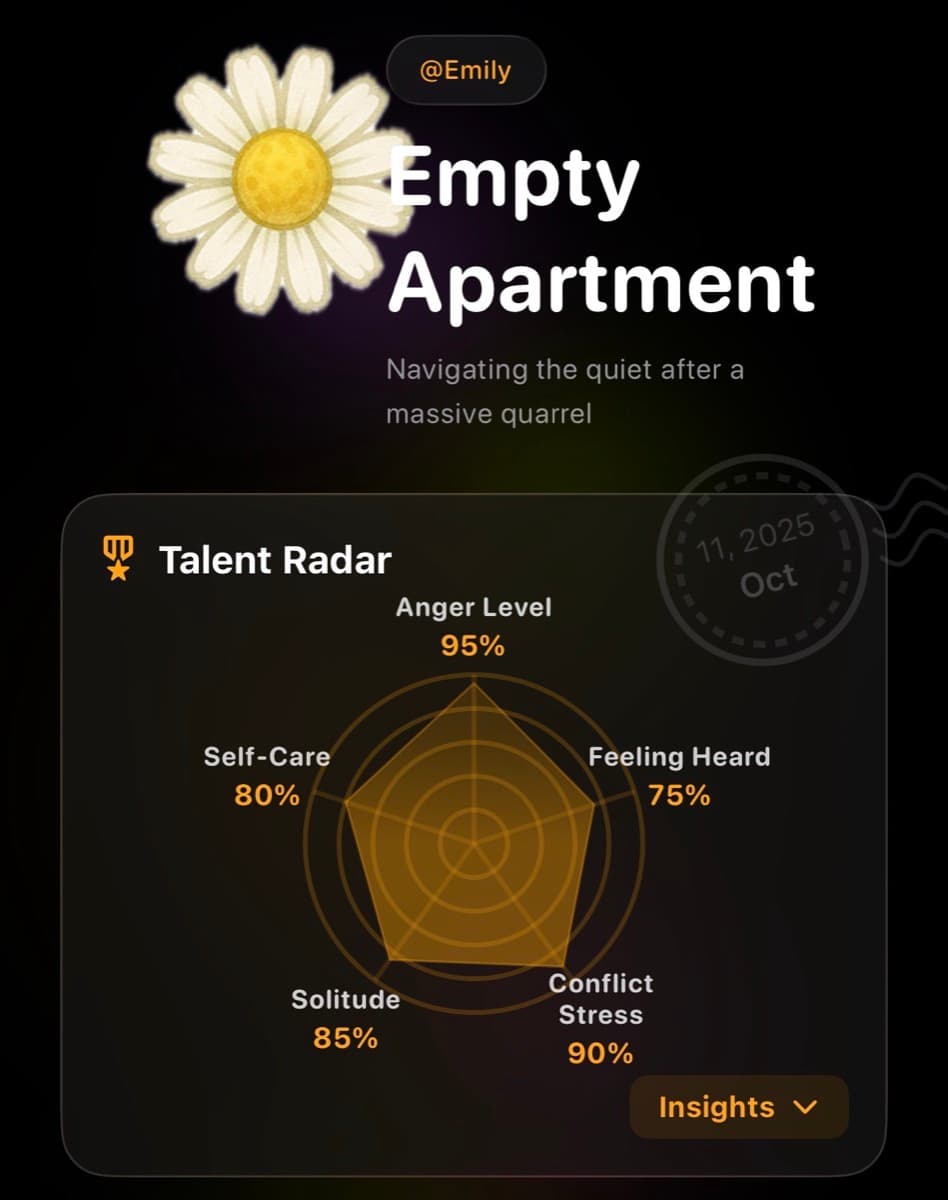
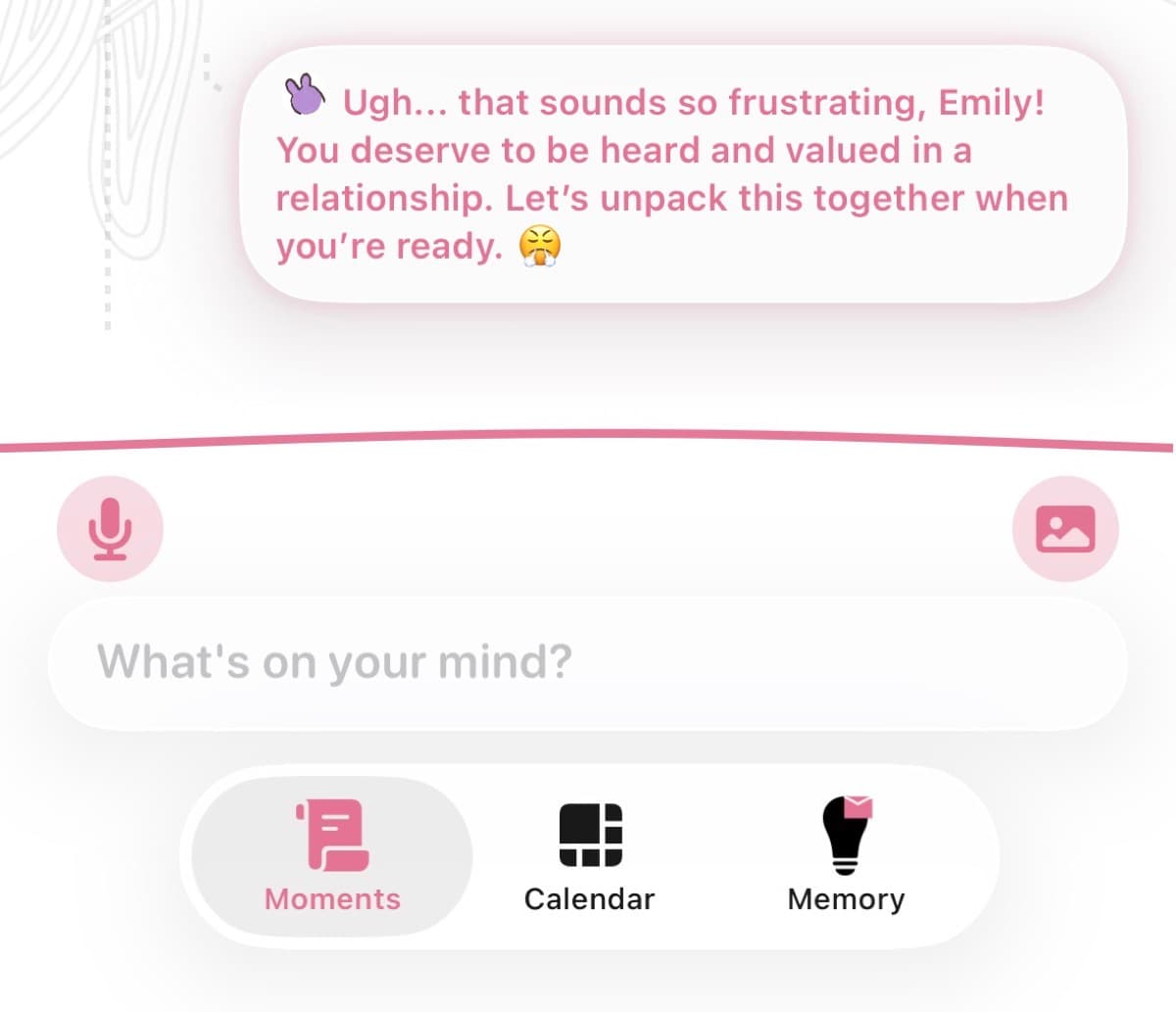
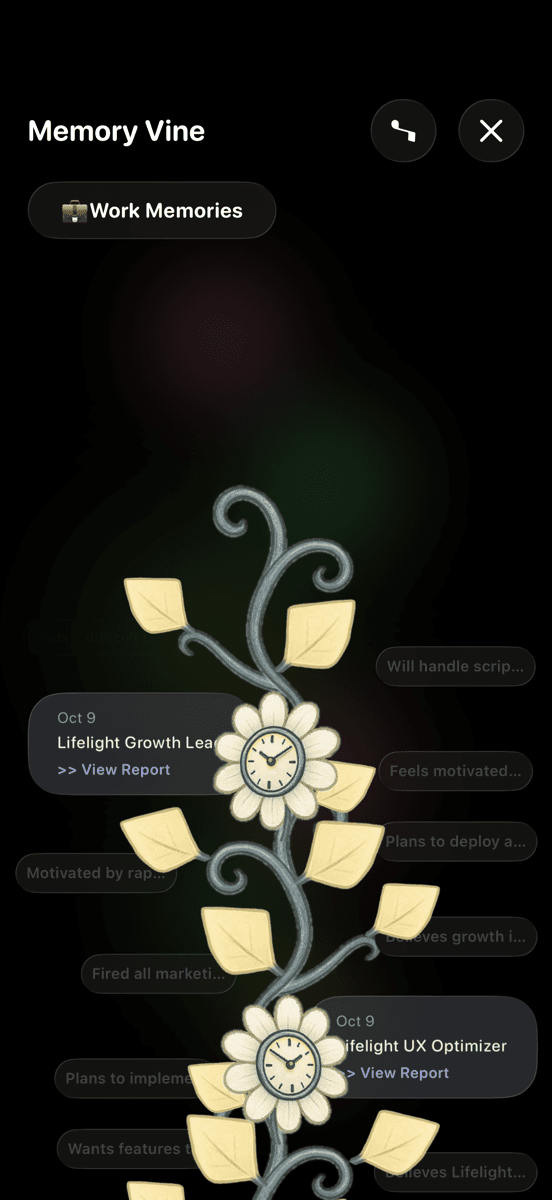
Using Lifelight to Track Sleep Patterns
When you're severely sleep-deprived, you often can't accurately assess how much sleep you're getting or how it's affecting mood. Lifelight helps identify patterns:
- Sleep tracking: Log sleep blocks (even fragmented ones) to see total hours
- Mood correlation: Notice connection between sleep and emotional state
- Symptom tracking: Track depression/anxiety symptoms alongside sleep data
- Share with doctor: "Here's my sleep log for the past month—I'm averaging 4.5 hours of fragmented sleep"
- Identify what helps: See if night shifts, medication, or sleep training improves sleep quality
When Baby Sleep Issues Require Help
Consider sleep consultation if:
- Baby over 4 months still waking every 1-2 hours
- You're experiencing mental health crisis due to sleep deprivation
- You've tried basic strategies without improvement
- Your relationship is suffering due to exhaustion
Sleep training isn't required: But if sleep deprivation is destroying your mental health, it's worth exploring all options without guilt.
For Partners: How to Support
If your partner is severely sleep-deprived:
- Implement night shifts immediately: Don't wait for them to ask
- Take over non-baby tasks: Cooking, cleaning, grocery shopping
- Don't suggest they "just nap": Offer specific sleep shift: "You sleep 9-2, I'll handle everything"
- Recognize mood changes as sleep deprivation: Not character flaws
- Consider hiring help: Night doula, postpartum support—worth every penny
The Timeline: When Does Sleep Improve?
Realistic expectations:
- 0-3 months: Survival mode. Sleep deprivation peaks. Focus on sleep shifts.
- 3-6 months: Some babies consolidate sleep; others don't. Consider gentle sleep interventions if needed.
- 6-12 months: Many babies sleep longer stretches (but not all—every baby different)
- 12+ months: Most parents sleeping more, though still disrupted
Important: If you're still severely sleep-deprived at 6+ months, this warrants medical attention for both you and baby.
You're Not Weak—You're Surviving Torture
Sleep deprivation is literally used as a torture method because it causes reliable psychological breakdown. We subject new parents to this and call it "normal."
It's not normal. It's not sustainable. And you don't have to accept it.
Prioritize sleep as aggressively as you'd treat any medical emergency. Ask for help. Lower your standards for everything else. Implement sleep shifts. Do whatever it takes.
Your mental health depends on it. Your baby needs a rested parent more than they need a perfect one.
Sleep isn't selfish. It's survival.