Three weeks after bringing your baby home, you're lying awake at 3 AM. The baby is finally sleeping, but you can't. Your heart is racing. Or maybe it's not racing—maybe you just feel... nothing. Empty. Detached.
You Google "postpartum depression" but the symptoms describe both everything and nothing you're experiencing. The advice is maddeningly vague: "Seek help if symptoms persist." But which symptoms? And help for what exactly?
Here's what nobody tells new parents: Postpartum depression and postpartum anxiety are different conditions that require different approaches—but 50% of women experience both simultaneously, making them incredibly difficult to distinguish.
This guide will help you identify what you're actually experiencing, why it matters, and how to get the right support for your specific symptoms.
The Critical Difference Nobody Explains
Postpartum Depression: The Fog of Emptiness
Core experience: Emotional numbness, detachment, hopelessness
What it actually feels like:
- You're going through the motions of caring for your baby, but feel disconnected from the experience
- Everything feels heavy, like you're moving through water
- You can't remember the last time you felt joy or excitement about anything
- Crying feels impossible, even when you want to—or you cry uncontrollably over small things
- Thoughts of escape ("What if I just left?") feel more appealing than thoughts of your baby
Postpartum Anxiety: The Storm of Hypervigilance
Core experience: Constant worry, racing thoughts, catastrophizing
What it actually feels like:
- You're checking if the baby is breathing multiple times per hour
- Your mind constantly generates worst-case scenarios (car crashes, SIDS, abduction)
- Physical symptoms: racing heart, chest tightness, difficulty breathing, nausea
- You can't sleep even when the baby sleeps because your mind won't stop
- Intrusive thoughts about something terrible happening to your baby
The Overlap Zone (Where 50% of Women Live)
Many women experience both conditions simultaneously—what researchers call "comorbid postpartum depression and anxiety." This creates a confusing experience:
"I feel completely numb and detached from my baby... but also terrified something will happen to him. I can't sleep because I'm worried, but I also don't care about anything. It makes no sense."
If this describes you, you're not confused—you're experiencing both conditions. This is actually more common than experiencing either alone.
The Diagnostic Questions That Actually Work
Instead of generic symptom checklists, ask yourself these specific questions:
For Depression:
- "If someone offered to watch the baby so I could do something I used to love, would I want to?"
Depression: No, nothing sounds appealing
Not depression: Yes, but I'm too anxious to leave - "When I look at my baby, what do I feel?"
Depression: Numbness, obligation, sometimes resentment
Not depression: Love mixed with worry/fear - "Can I imagine feeling happy again?"
Depression: No, the future looks gray and hopeless
Not depression: Yes, if these worries would just stop
For Anxiety:
- "What's the primary emotion when caring for the baby?"
Anxiety: Fear, constant vigilance, "what if" thoughts
Not anxiety: Emptiness, disconnection, going through motions - "Why can't I sleep when the baby sleeps?"
Anxiety: Mind racing with worries and scenarios
Not anxiety: Don't care enough to sleep, or sleeping excessively - "Would I feel better if someone could guarantee the baby's safety?"
Anxiety: Yes, that's my biggest fear
Not anxiety: No, that's not really the problem
Why This Distinction Matters for Treatment
Treatment for Postpartum Depression:
- Medication: SSRIs (Zoloft, Prozac)—safe while breastfeeding
- Therapy: Interpersonal therapy (IPT), cognitive behavioral therapy (CBT)
- Lifestyle: Light therapy, exercise (when energy allows), social connection
- Timeline: 6-8 weeks to see medication effects, 8-12 weeks for therapy benefits
Treatment for Postpartum Anxiety:
- Medication: SSRIs, sometimes short-term benzodiazepines (with caution)
- Therapy: Exposure therapy, mindfulness-based stress reduction, CBT for anxiety
- Skills: Breathing exercises, grounding techniques, worry scheduling
- Timeline: Anxiety responds faster—skills can help within days, medication within 2-4 weeks
Treatment for Both (Comorbid Presentation):
- Usually SSRIs (which treat both conditions)
- Therapy addressing both numbness AND hypervigilance
- Skills for managing anxiety while addressing underlying depression
- May require medication adjustment as one condition improves before the other
What to Tell Your Doctor
Instead of "I think I have postpartum depression," try these specific statements:
If primarily depression:
"I feel emotionally numb and disconnected from my baby. I'm not enjoying anything, and I can't imagine feeling better. I'm functioning, but everything feels hollow."
If primarily anxiety:
"I'm constantly worried something terrible will happen to my baby. I can't sleep because my mind won't stop racing with worst-case scenarios. I'm checking on the baby excessively and having intrusive thoughts about harm."
If both:
"I'm experiencing both emotional numbness and constant anxiety. I feel detached from my baby but also terrified something will happen to them. I can't sleep because of worry, but I also feel hopeless about the future."
The "Baby Blues" vs. Actual Disorders
Baby blues (60-80% of women, not a disorder):
- Starts 2-3 days after birth
- Resolves within 2 weeks
- Mood swings, crying, irritability
- Doesn't interfere with functioning
- No treatment needed—support and rest are sufficient
Postpartum depression/anxiety (15-20% of women):
- Can start anytime in first year (peak at 6-8 weeks)
- Doesn't improve without intervention
- Interferes with daily functioning and bonding
- Requires professional treatment
The 2-week rule: If symptoms persist beyond 2 weeks postpartum or start getting worse instead of better, seek evaluation. Don't wait to "see if it gets better"—early intervention prevents escalation.
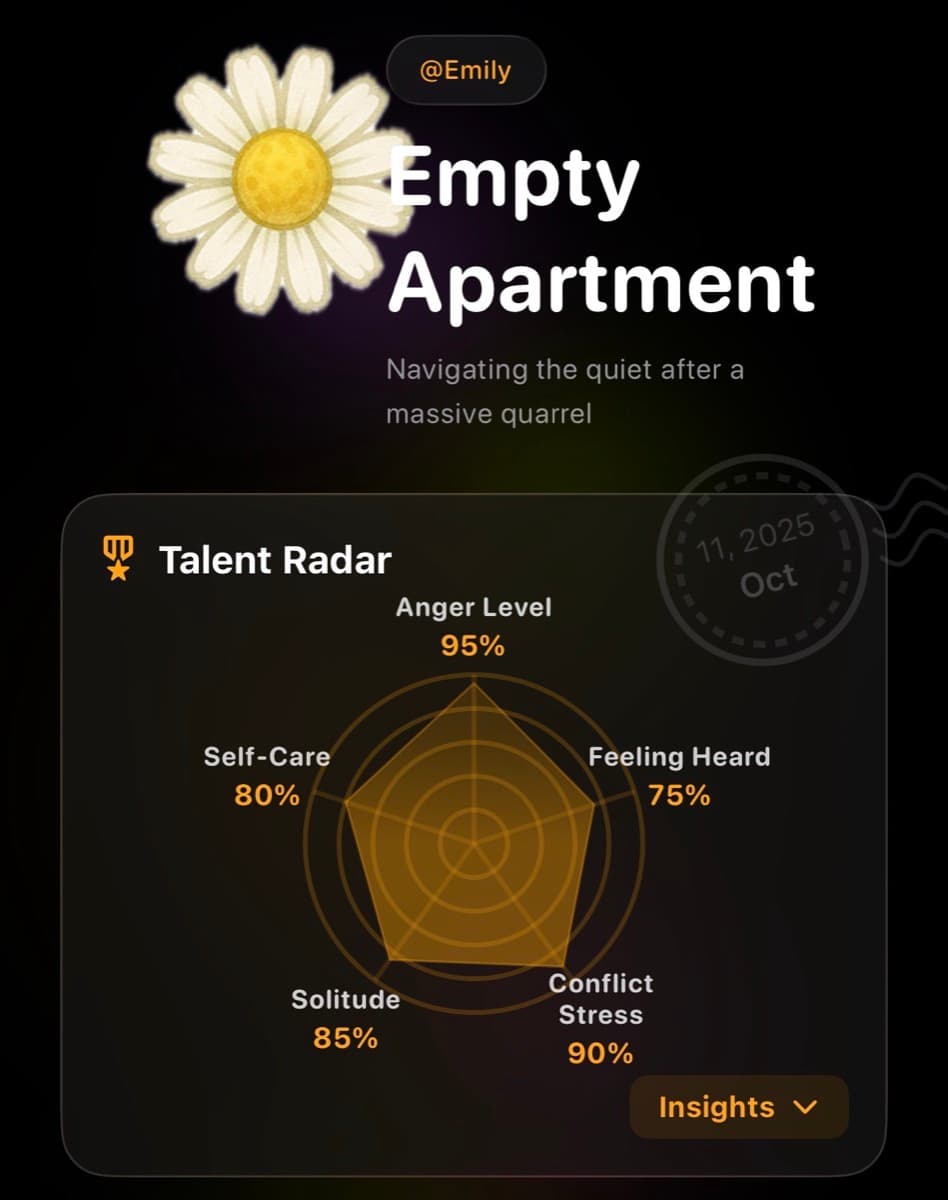
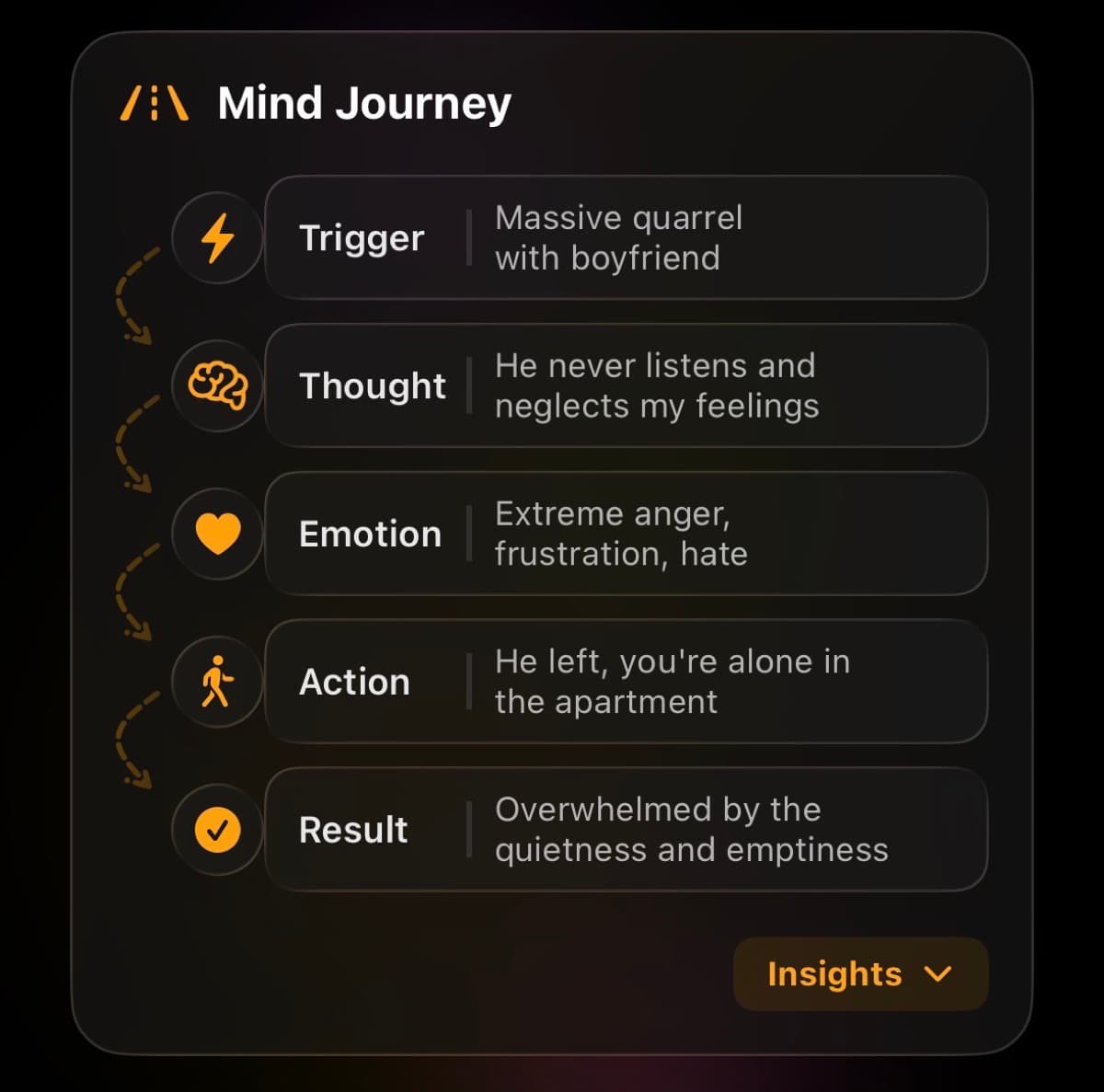
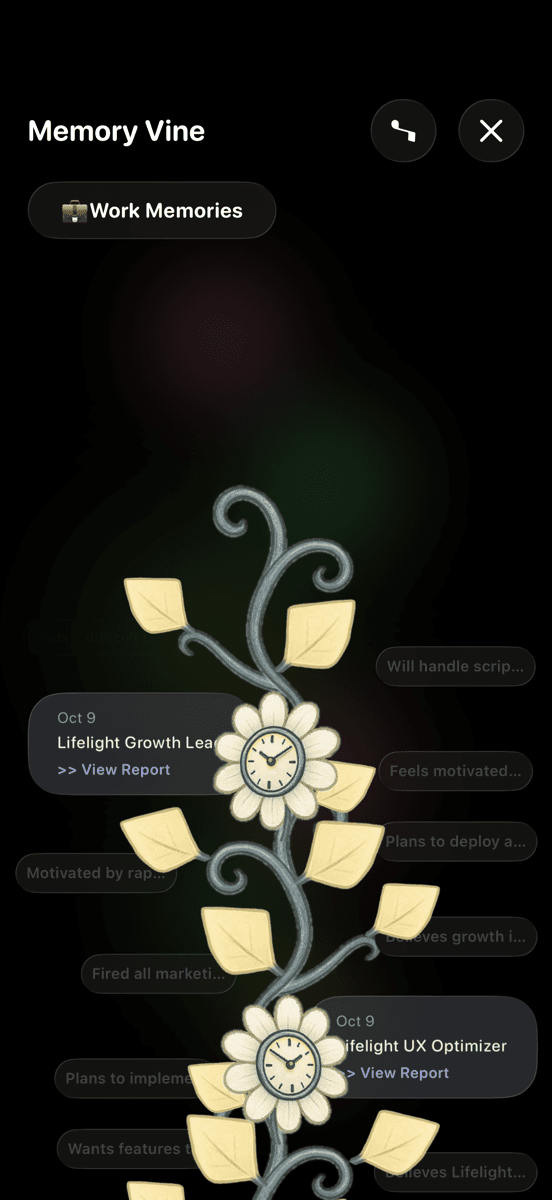
Lifelight for Postpartum Mental Health Tracking
Many new parents struggle to articulate their mental health to doctors during brief appointments. Lifelight helps you track patterns that matter:
- Mood tracking: Document emotional numbness vs. anxiety patterns over weeks
- Sleep vs. worry: Track whether insomnia is from inability to sleep (depression) or racing thoughts (anxiety)
- Intrusive thoughts: Privately journal about disturbing thoughts to share with providers
- Treatment response: Monitor whether medication helps numbness, anxiety, or both
- Emma AI support: Get immediate coping strategies for 3 AM anxiety spirals or moments of deep disconnection
Lifelight creates a documented record you can show your doctor: "Here's my mood over the past 4 weeks—see how it's not improving?" This concrete data often leads to better, faster treatment.
Emergency Warning Signs (Call Your Doctor Today)
Seek immediate help if you experience:
- Thoughts of harming yourself or your baby
- Inability to care for yourself or baby
- Panic attacks lasting more than 30 minutes
- Hallucinations or delusions (seeing/believing things that aren't real)
- Feeling detached from reality
These are signs of postpartum psychosis (rare but serious) or severe postpartum depression/anxiety requiring immediate intervention.
The Timeline Nobody Mentions
Without treatment:
- Postpartum depression averages 7+ months if untreated
- Postpartum anxiety can persist for years
- Both increase risk of chronic depression/anxiety beyond postpartum period
With treatment:
- Most women see significant improvement within 8-12 weeks
- Anxiety symptoms often improve faster than depression
- Early intervention (within first 3 months) prevents chronic conditions
What Recovery Actually Looks Like
From depression:
- Colors start looking brighter again (literally—depression affects visual processing)
- Small moments of joy when looking at your baby
- Energy to do things beyond basic survival
- Ability to imagine a future that doesn't feel gray
From anxiety:
- Ability to sleep when baby sleeps without checking constantly
- Intrusive thoughts become less frequent and easier to dismiss
- Physical symptoms (racing heart, chest tightness) decrease
- Can leave baby with trusted caregiver without panic
You're Not Failing at Motherhood
Postpartum depression affects 1 in 7 women. Postpartum anxiety affects 1 in 10. Combined? Even more common.
These are medical conditions caused by hormonal shifts, sleep deprivation, and neurobiological changes—not character flaws or failures of willpower.
Seeking help isn't admitting defeat. It's the strongest thing you can do for yourself and your baby.
Your baby doesn't need a perfect mother. They need a healthy mother who's getting support. You deserve to feel better. And you will.