Your maternity leave ends in two weeks. Everyone keeps asking if you're excited to go back to work, to "get back to normal," to have "adult conversations" again.
But you're not excited. You're grieving.
You're grieving the hours you'll miss with your baby. You're terrified of leaving them with someone else. You're worried you won't be able to pump enough. You're anxious about how you'll possibly perform at work while sleep-deprived and emotionally wrecked.
And underneath all of that? Guilt. Soul-crushing guilt for feeling torn. Guilt for wanting to keep your career. Guilt for leaving your baby. Guilt for not being enough in either place.
Here's what nobody tells you: Returning to work postpartum is one of the hardest transitions you'll ever make—and it's happening at the exact moment when you're most vulnerable.
This guide covers the emotional reality, practical strategies, and mental health impacts of returning to work after having a baby.
The Numbers That Show How Broken the System Is
- 67% of US mothers return to work within 3 months of giving birth
- 23% have ZERO paid leave—they're back within 2 weeks
- The US is the only developed nation without mandatory paid parental leave
- Mothers who return before 12 weeks have 3x higher rates of postpartum depression
- Breastfeeding rates drop dramatically when mothers return to work early (not due to choice, but lack of pumping support)
You're not struggling because you're weak. You're struggling because you're trying to function in a system designed to make this impossible.
The Emotional Stages of Returning to Work
Stage 1: Anticipatory Grief (Weeks Before Return)
What it feels like:
- Counting down days with dread
- Crying when thinking about leaving baby
- Guilt for "abandoning" your baby (you're not—but the feeling is real)
- Anxiety about childcare safety
- Feeling like you "should" be grateful to have a job, which makes guilt worse
Why it happens: You're anticipating loss—loss of time, loss of control, loss of the identity you've been building for weeks/months as primary caregiver.
Stage 2: The First Week (Crisis Mode)
What it feels like:
- Overwhelming urge to turn around and go home
- Constantly checking phone for daycare updates
- Unable to focus on work
- Crying in bathroom/car
- Physical pain from missing baby (and from engorged breasts if pumping)
What helps: Lower all expectations. Your only goal this week is survival—not productivity, not performance, just showing up.
Stage 3: The Adjustment (Weeks 2-8)
What it feels like:
- Slightly less crying, but still regular waves of grief
- Developing routines (pumping schedule, pickup/dropoff)
- Exhaustion from juggling everything
- Frustration that you can't fully commit to work OR home
- Occasional moments where work feels like a relief (followed by guilt for feeling that)
Why it's hard: You're learning to live in the tension of being two places at once—physically at work, emotionally with baby.
Stage 4: The New Normal (Months 3+)
What it feels like:
- Still hard, but no longer crisis-level
- Routines feel more automatic
- Able to focus at work for periods of time
- Guilt shifts from constant to situational (triggered by missed milestones, sick days)
- Acceptance that this is your reality (not the same as liking it)
The Pumping Reality Nobody Prepares You For
What they tell you:
"You're legally entitled to pumping breaks!"
What actually happens:
- Pumping room is a converted closet: Uncomfortable, depressing, or nonexistent
- Time pressure: Rushing through pumping sessions, not fully emptying, supply drops
- Meeting conflicts: "Can't you just pump later?" (No, that's not how breasts work)
- Judgment: Eye rolls, comments about "special treatment," resentment from colleagues
- Equipment failures: Forgotten parts, broken pumps, spilled milk
- Emotional toll: Pumping while looking at baby photos, crying over pump flanges
Practical pumping strategies:
- Block pumping time on calendar: Treat it like unmissable meetings
- Backup supplies at work: Extra pump parts, batteries, milk storage bags
- Know your rights: PUMP Act requires break time and private space (not bathroom)
- Let go of perfectionism: If supply drops, it's not your failure—it's the system's
- Consider your options: Formula supplementation isn't failure; combo feeding is valid
Managing the Identity Crisis
Before baby:
Work was a huge part of your identity. You were competent, productive, valued.
During maternity leave:
You built new identity as mother. Your baby's needs were primary focus.
Returning to work:
You're expected to be both identities simultaneously—and feel like you're failing at both.
The impossible standard:
- Perform at work as if you don't have a baby
- Parent as if you don't have a job
- Never let either side see the strain
The reality: You're one person doing two full-time jobs. Something has to give. That's not failure—that's physics.
The Mental Health Impact
Returning to work increases risk of:
- Postpartum depression: Especially if return is before 12 weeks
- Anxiety: Constant worry about baby, childcare, performance
- Burnout: Juggling work + parenting with no recovery time
- Relationship strain: Division of labor conflicts, resentment
- Loss of breastfeeding relationship: Grief when pumping/feeding ends sooner than desired
Warning signs you need help:
- Constant crying or inability to stop crying when thinking about baby
- Panic attacks during work or dropoff
- Inability to focus on work due to intrusive thoughts
- Feeling detached from baby when you are together
- Rage at partner, coworkers, or childcare providers
- Thoughts of quitting job impulsively (even if financially unrealistic)
- Physical symptoms: insomnia, digestive issues, constant illness
If experiencing 3+ of these, seek professional evaluation for postpartum depression/anxiety.
Childcare Guilt: The Emotion Nobody Validates
The guilt thoughts:
- "Someone else is seeing my baby's first steps/words"
- "My baby cries when I drop them off—they must think I'm abandoning them"
- "The daycare provider spends more waking hours with my baby than I do"
- "I'm missing so much—am I even their parent anymore?"
The reality check:
- Your baby knows you're their parent: Attachment isn't about quantity of hours; it's about quality of connection
- Crying at dropoff is normal: And usually stops within 5 minutes (ask for video proof if helps)
- Childcare providers are caregivers, not replacements: They provide care; you provide irreplaceable parental love
- Your baby benefits from your wellbeing: A financially stable, mentally healthy parent is better than a burned-out, resentful one
Practical Survival Strategies
1. Lower ALL Standards Temporarily
At work:
- Aim for "good enough," not excellence
- Say no to extra projects
- Use all shortcuts (templates, delegation, simplified processes)
At home:
- Survival meals (frozen, takeout, meal delivery)
- Lower cleaning standards dramatically
- Outsource whatever you can afford (cleaning service, grocery delivery)
2. Build in Connection Rituals
- Morning cuddle time: Even 10 minutes of focused connection before leaving
- Reunion ritual: Immediate 15 minutes of floor time when you get home (before anything else)
- Bedtime routine: Non-negotiable quality time
- Weekend priority: One-on-one time takes precedence over chores
3. Communicate with Employer
What to negotiate:
- Gradual return (part-time first few weeks if possible)
- Flexibility for childcare emergencies
- Protected pumping time
- Work-from-home days if possible
- Adjusted deadlines initially
How to frame it: Not as asking for special treatment, but as transition plan that ensures you can return to full productivity sustainably.
4. Partner Division of Labor
Common conflict: Partner doesn't understand how much mental/emotional labor you're carrying.
Solution: Explicit division of all tasks—not just physical tasks, but mental load too:
- Who schedules pediatrician appointments?
- Who handles daycare communication?
- Who plans meals?
- Who does laundry, including remembering when it needs to be done?
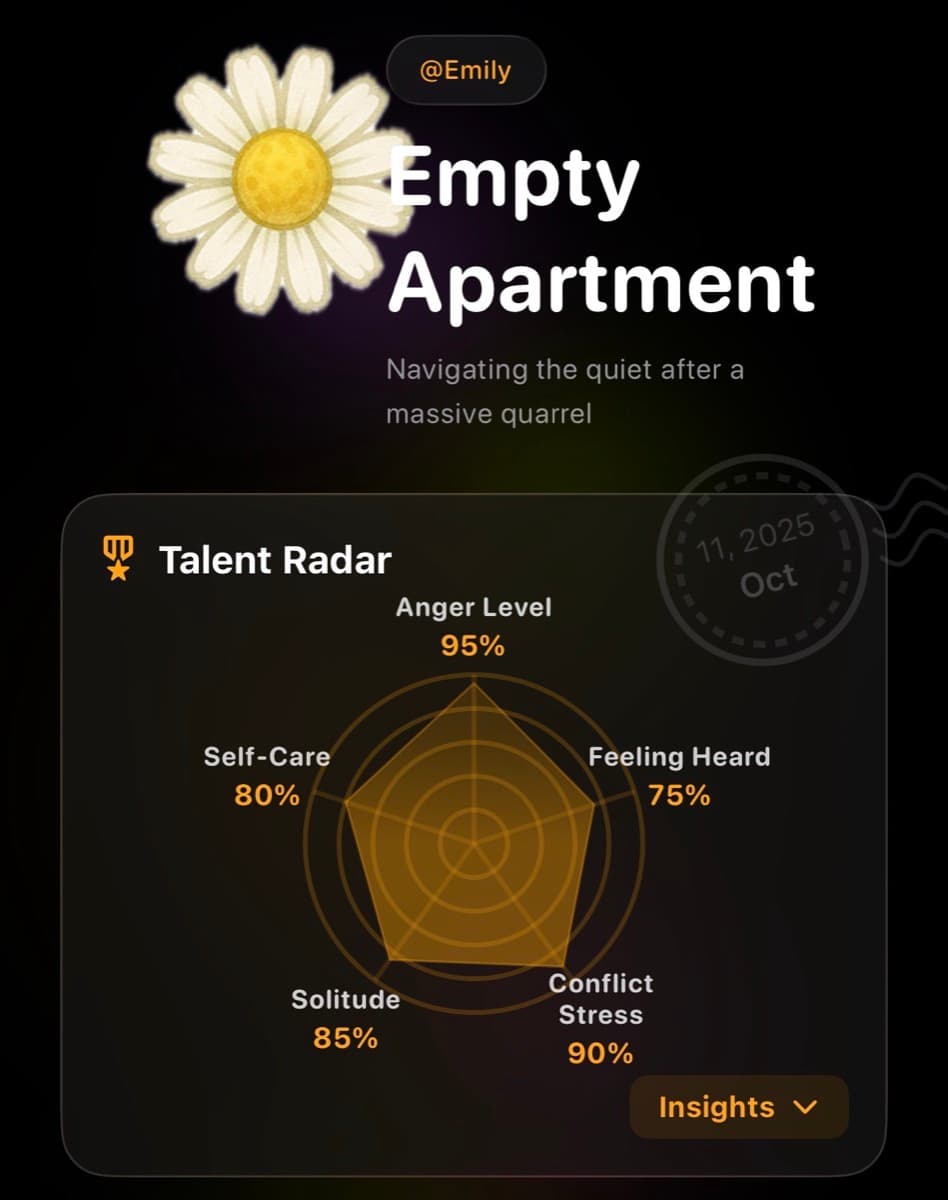
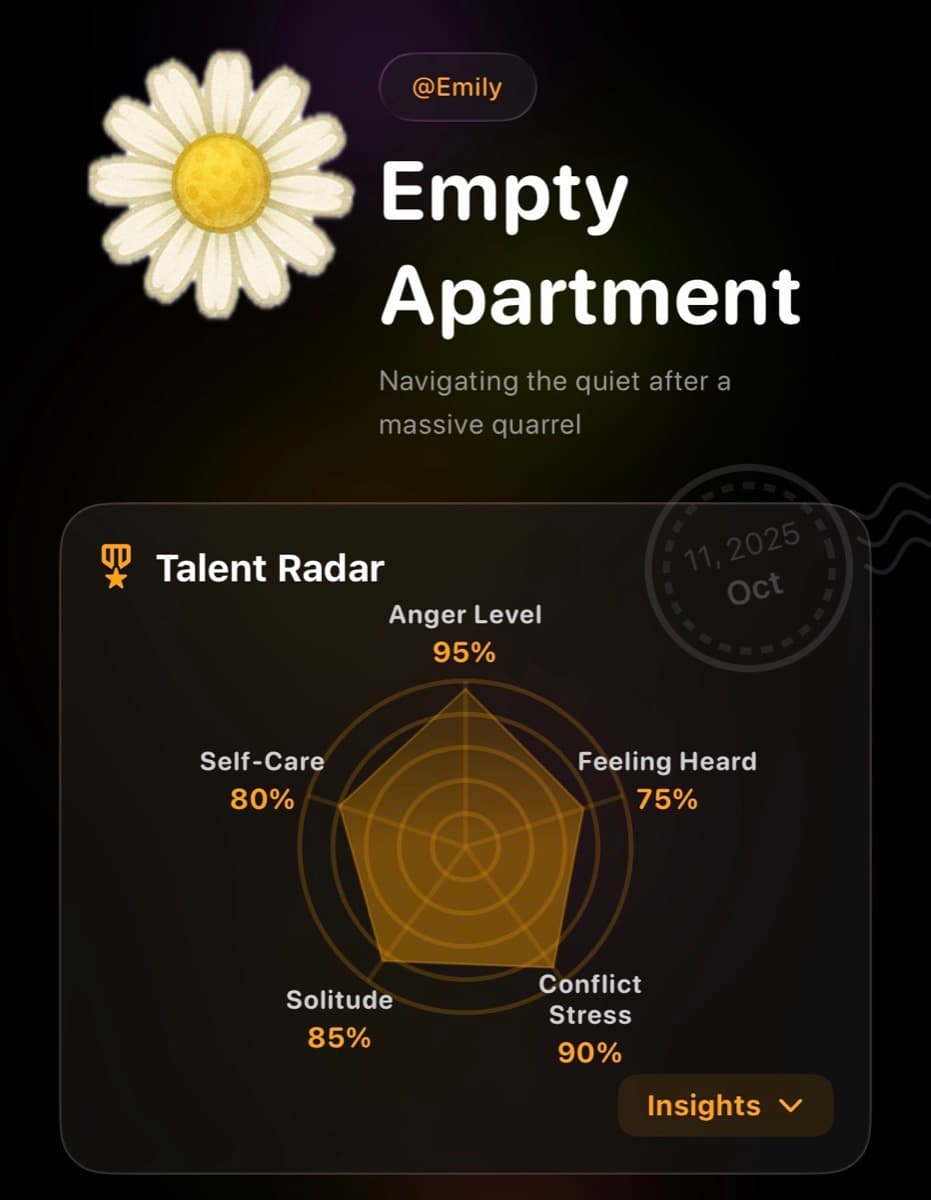
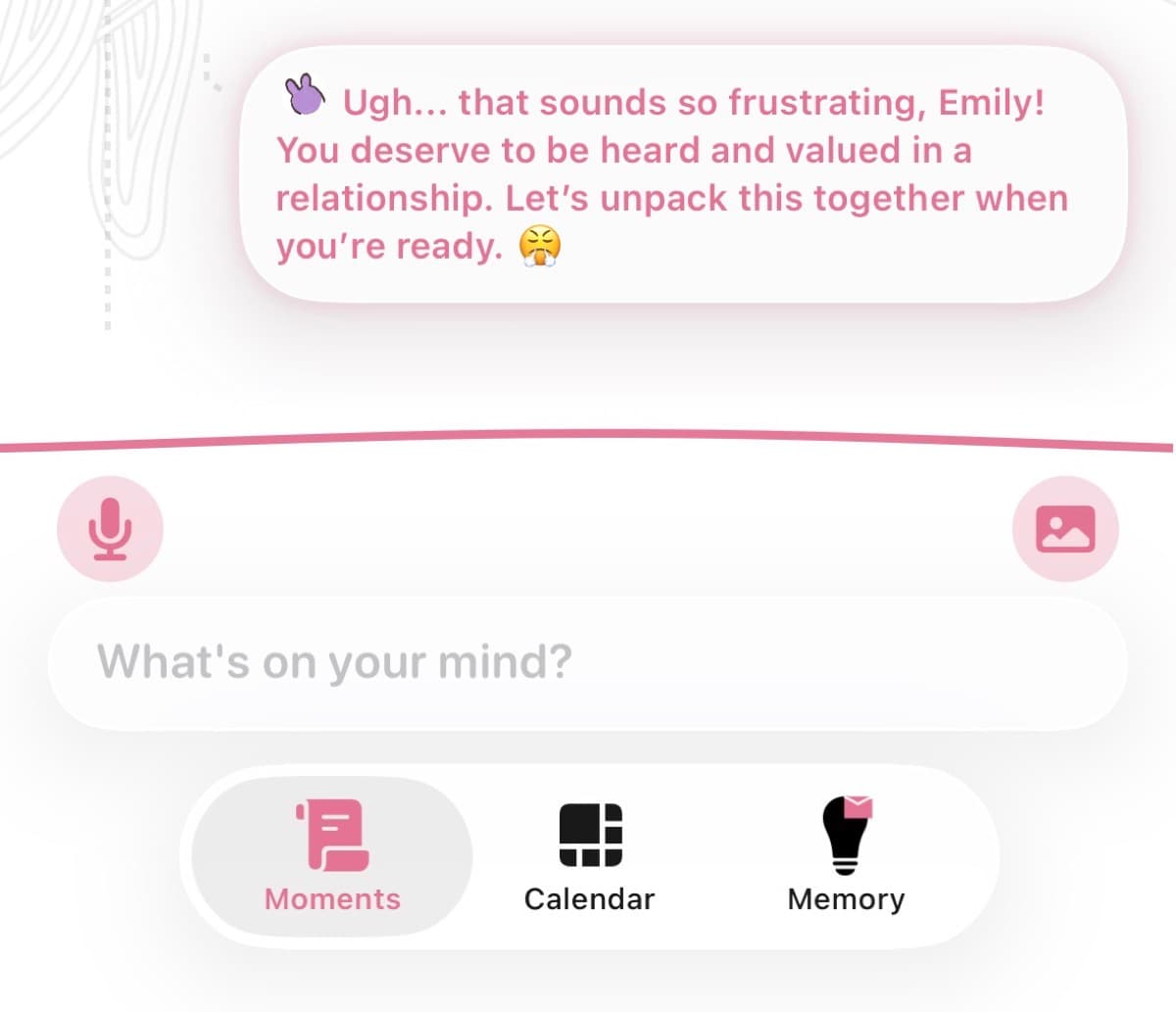
Using Lifelight to Navigate Return to Work
The transition back to work triggers intense emotions that are hard to process in real-time. Lifelight helps you track and manage mental health:
- Mood tracking: Notice if depression/anxiety symptoms increase after return to work
- Trigger identification: Track what situations cause most distress (dropoff, missed milestones, pumping)
- Pattern recognition: See if there are better/worse days of week, times of day
- Private journaling: Process guilt, grief, and ambivalence without judgment
- Emma AI support: Get coping strategies for acute distress moments (crying in bathroom at work)
- Share with therapist: Concrete data about emotional patterns informs treatment
When to Consider Making a Change
It might be time to reconsider your work situation if:
- Your mental health is deteriorating despite treatment
- You're spending more on childcare than you're earning
- Your employer is hostile to basic accommodations (pumping, sick child)
- You're experiencing suicidal thoughts or severe depression
- Your relationship is crumbling from the stress
Options to explore:
- Part-time work or reduced hours
- Remote work arrangements
- Job change to more family-friendly employer
- Career pause (if financially feasible)
- Shifting to partner's insurance/income while you recover
Important: Don't make major decisions during first 8 weeks back. Give yourself adjustment period before deciding if situation is unsustainable.
For Partners: How to Support
If your partner is struggling with return to work:
- Validate the grief: "This is really hard" > "At least you have a good job"
- Take on more at home: First weeks back, they need maximum support
- Handle morning routine: Taking over getting baby ready reduces morning stress
- Don't minimize guilt: Guilt is irrational but very real; acknowledge it
- Encourage professional help: If you see signs of PPD/anxiety
What Recovery Looks Like
You'll know you're adjusting when:
- You can think about work without constant intrusive thoughts about baby
- Dropoff gets easier (still not fun, but not devastating)
- You have moments of genuine engagement with work
- Guilt shifts from constant to situational
- You find new rhythm and routines that work
- You can enjoy time with baby without anxious thoughts about work
Timeline: Most people feel significantly better by 2-3 months back. If you don't, that's a sign to seek additional support.
You're Not Failing—The System Is
Returning to work 6-12 weeks after giving birth—while sleep-deprived, hormonally fluctuating, possibly still bleeding, and newly bonded with a baby—is inhumane.
You're not struggling because you're weak. You're struggling because you're trying to do the impossible.
Be gentle with yourself. Lower your standards. Ask for help. Prioritize your mental health.
Your baby needs a healthy parent more than they need a perfect one. And you deserve support during one of the hardest transitions of your life.
It gets easier. Not easy—but easier.