Your partner just had a baby three months ago. She's struggling with postpartum depression, and you're doing everything you can to support her—taking night shifts, handling household tasks, being the "strong one."
But lately, you've been feeling... off. Irritable. Disconnected. You love your baby, but you don't feel the overwhelming joy everyone talks about. You're exhausted, anxious, and sometimes resentful of how much your life has changed.
You Google "new parent stress" but everything is about mothers. You must just need to toughen up, right? Your partner birthed the baby—you have no right to struggle.
Here's what nobody tells you: 10% of new fathers and non-birthing partners experience postpartum depression. When the birthing partner has PPD, that number jumps to 50%. You're not weak. You're experiencing a real, documented condition—one that almost no one talks about.
Why Partner Postpartum Depression Is Invisible
The cultural narrative:
- "Real men don't get depressed about becoming fathers"
- "You didn't give birth—you can't have postpartum depression"
- "Your partner needs support; your feelings don't matter right now"
- "Just be grateful you have a healthy baby"
Result: Male partners experiencing depression feel guilty, ashamed, and invisible. They don't seek help. And their families suffer.
What Partner PPD Actually Looks Like
Partner postpartum depression often manifests differently than maternal PPD:
In Women (More Likely):
- Sadness, crying, emotional expression
- Anxiety about baby's health and safety
- Difficulty bonding with baby
In Men/Non-Birthing Partners (More Likely):
- Irritability and anger: Snapping at partner, road rage, short fuse
- Withdrawal: Working longer hours, avoiding home, emotional distance
- Risk-taking behavior: Increased alcohol use, reckless driving, impulsive decisions
- Physical symptoms: Headaches, digestive issues, chronic fatigue
- Feeling trapped or resentful: Grief for old life, feeling like freedom is gone
The invisible depression: Because it doesn't look like stereotypical sadness, it's often dismissed as "stress" or "adjustment" rather than recognized as clinical depression.
The Risk Factors Nobody Mentions
You're at higher risk if:
- Your partner has postpartum depression: Single biggest predictor (50% correlation)
- History of depression/anxiety: Personal or family history increases risk
- Relationship conflict: Pre-existing strain in partnership
- Financial stress: Pressure to provide, lost income, new expenses
- Unplanned pregnancy: Ambivalence about parenthood
- Lack of social support: Isolation from friends, no parental leave
- Sleep deprivation: Less than 5 hours sleep consistently
- Identity loss: Entire life revolves around baby, losing sense of self
The Hormonal Connection
Yes, men and non-birthing partners experience hormonal changes too:
- Testosterone drops: 20-30% decrease in testosterone after baby arrives
- Cortisol increases: Chronic stress hormone elevation from sleep deprivation
- Oxytocin fluctuations: Bonding hormone changes affect mood and attachment
- Prolactin increases: Nurturing hormone rises (yes, in men too) affecting mood
This isn't "all in your head"—it's neurobiological.
The Impact on the Whole Family
When partner PPD goes untreated:
- Child outcomes: Children of depressed fathers show higher rates of behavioral problems, emotional dysregulation, and developmental delays
- Relationship strain: Conflict increases, satisfaction plummets, divorce risk rises
- Maternal depression worsens: Partners unable to provide support, creating downward spiral
- Long-term effects: Partner depression in infancy predicts ongoing mental health issues years later
Your mental health isn't selfish—it's essential for your family's wellbeing.
The Questions to Ask Yourself
Instead of generic depression screenings designed for women, ask these specific questions:
- "Am I irritable more than I'm sad?"
Partner PPD often manifests as anger rather than sadness - "Am I avoiding going home or spending time with my family?"
Withdrawal and escape behaviors are key signs - "Am I drinking/working/gaming more than before the baby?"
Men often self-medicate depression through behavior rather than recognizing it as mood disorder - "Do I feel trapped or resentful about my new life?"
Ambivalence doesn't mean you're a bad parent—it can signal depression - "Am I constantly worried about money/providing?"
Excessive financial anxiety beyond normal concern - "Do I feel like I'm failing as a partner/parent?"
Persistent feelings of inadequacy
If you answered yes to 3 or more, consider seeking evaluation.
Treatment Approaches
Therapy (Most Effective):
- CBT (Cognitive Behavioral Therapy): Addresses negative thought patterns and behaviors
- Couples therapy: Often essential since partner dynamic affects both people's mental health
- Men's support groups: Connecting with other new fathers reduces isolation
Finding the right therapist matters: Look for someone experienced with men's mental health and postpartum issues specifically
Medication:
- Same SSRIs used for maternal PPD (Zoloft, Prozac, etc.)
- Often men are more resistant to medication due to stigma
- 6-8 weeks to see full effects
- Can be combined with therapy for best outcomes
Lifestyle Interventions:
- Sleep (non-negotiable): Trade night shifts with partner so each person gets one 4-5 hour stretch
- Exercise: 30 minutes of activity as effective as medication for mild-moderate depression
- Social connection: Regular contact with friends (doesn't have to be about baby)
- Maintain identity: Keep at least one pre-baby hobby/activity
- Parental leave if possible: Time to bond and adjust reduces PPD risk
For the Struggling Partner: What to Do Now
1. Name it:
"I think I'm experiencing postpartum depression." Saying it out loud to your partner, friend, or doctor is the first step.
2. Talk to your partner:
Use specific language:
"I'm struggling more than I expected with the transition to parenthood. I think I need professional help. Can we figure out how to make that work?"
3. Find support:
- Postpartum Support International: 1-800-944-4773 (for all parents, not just mothers)
- Local new parent groups (many now include partner-specific groups)
- Online communities for new fathers
4. Be honest with your doctor:
Many doctors don't screen partners for PPD. You may need to advocate for yourself:
"I'm experiencing irritability, withdrawal, and feeling disconnected from my family. I'd like to be screened for postpartum depression."
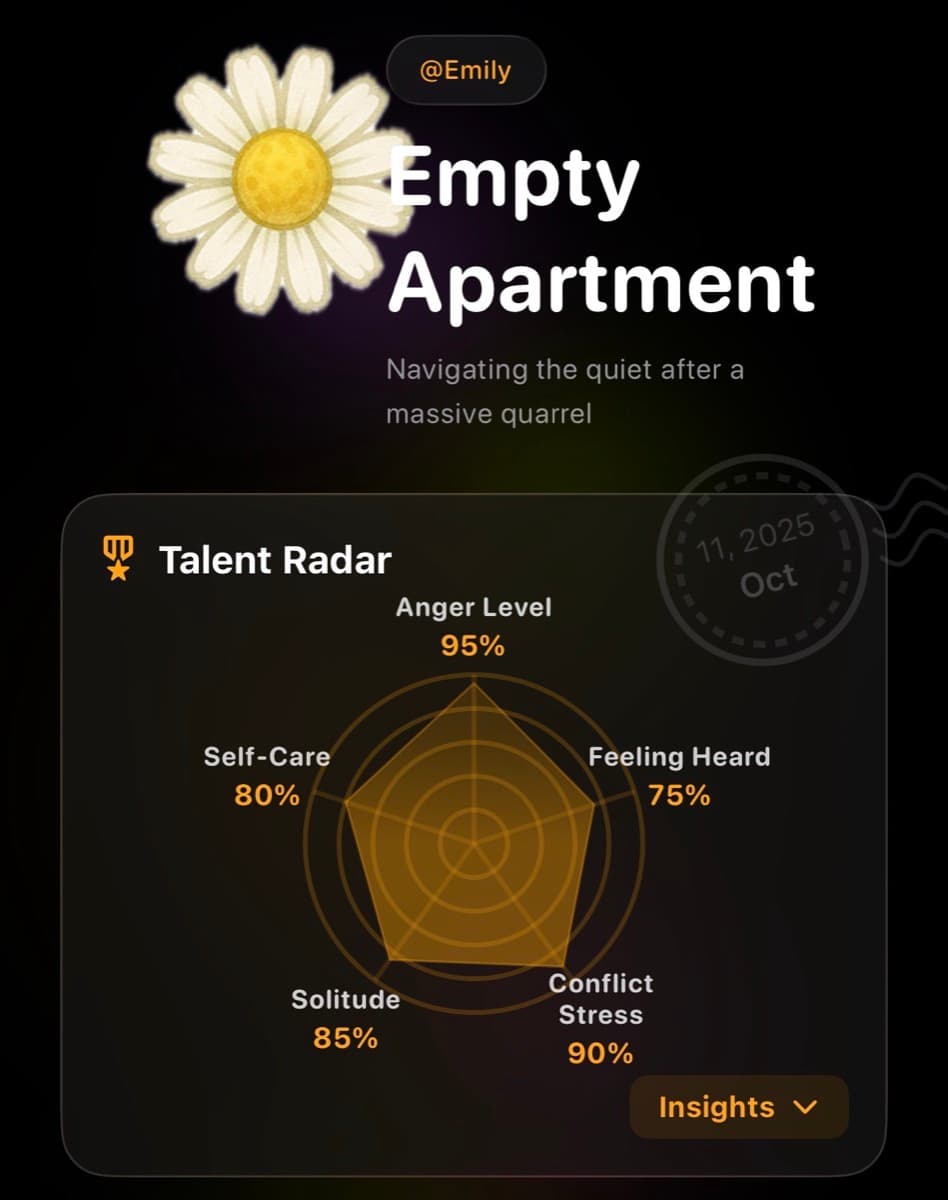
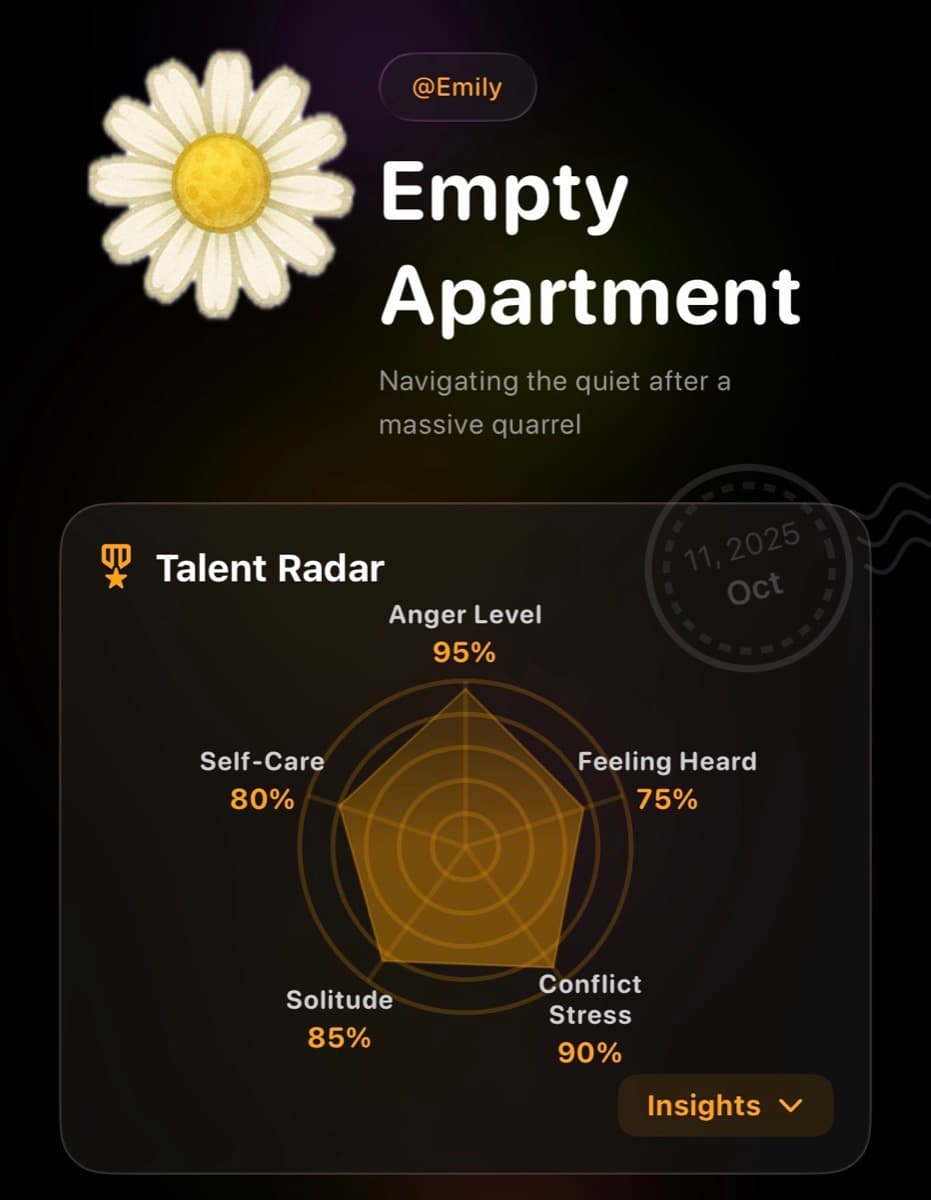
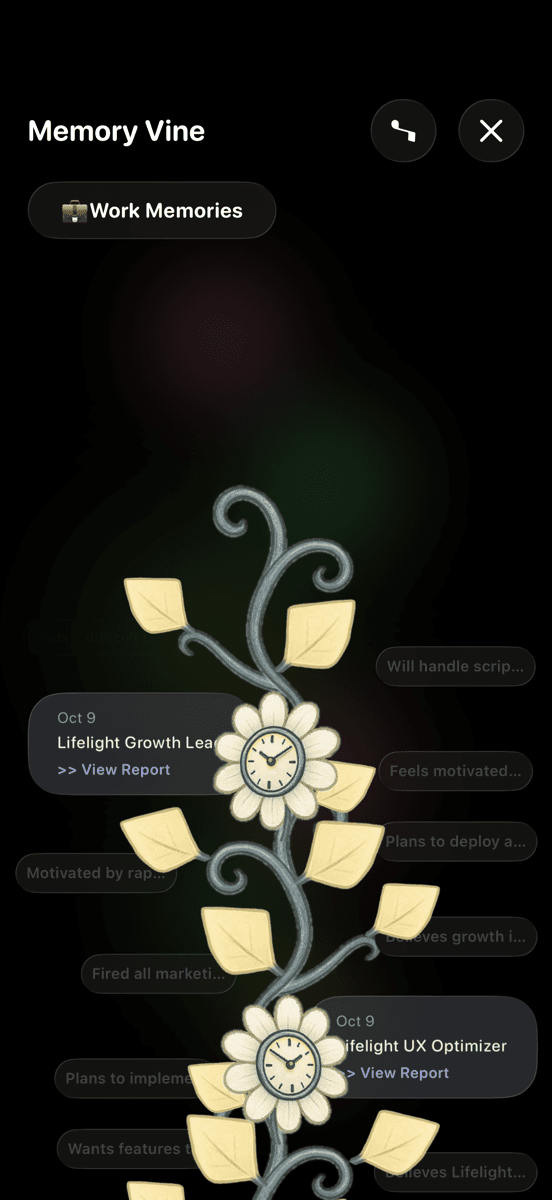
Using Lifelight to Track Partner PPD
Many men struggle to articulate mood changes or recognize patterns. Lifelight helps track what matters:
- Irritability tracking: Notice if anger is increasing over time vs. isolated bad days
- Sleep correlation: See connection between sleep deprivation and mood
- Withdrawal patterns: Track avoidance behaviors (working late, drinking, screen time)
- Treatment response: Monitor whether therapy/medication is actually helping
- Share with partner: Concrete data helps your partner understand what you're experiencing
- Emma AI: Private space to process feelings you're not ready to say out loud yet
For Partners of Someone with PPD
What helps:
- Recognize it's a medical condition: Not laziness, weakness, or lack of love for you/baby
- Encourage treatment without nagging: "I noticed you've been really stressed. Would talking to someone help?"
- Don't take irritability personally: It's a symptom, not a reflection of your relationship
- Share parenting load: Don't assume you have to do everything because they're struggling
- Get your own support: You can't pour from an empty cup
What doesn't help:
- "Just be grateful we have a healthy baby"
- "I'm struggling too—you need to step up"
- "Real men don't get depressed"
- "You don't have postpartum depression—you didn't give birth"
The Cultural Shift We Need
Partner postpartum depression will remain invisible until we:
- Screen all new parents: Not just birthing mothers, but partners too
- Normalize partner mental health: PPD isn't just a "mom issue"
- Provide paid parental leave: Financial stress and lack of bonding time increase risk
- Recognize male depression looks different: Irritability and withdrawal are depression symptoms
- Create partner-specific resources: Most support groups/materials assume female experience
Recovery Is Possible
With treatment, most partners see significant improvement within 8-12 weeks. The fog lifts. Connection to your baby and partner strengthens. Life starts feeling manageable again.
You're not failing at fatherhood. You're experiencing a medical condition that affects 1 in 10 new fathers. Seeking help isn't weakness—it's the strongest thing you can do for your family.
Your mental health matters. Your experience is valid. You deserve support.
Get help. You'll be glad you did.